Care coordination for improved outcomes for unsheltered
Margaret Adams, Corporation for Supportive Housing
Background
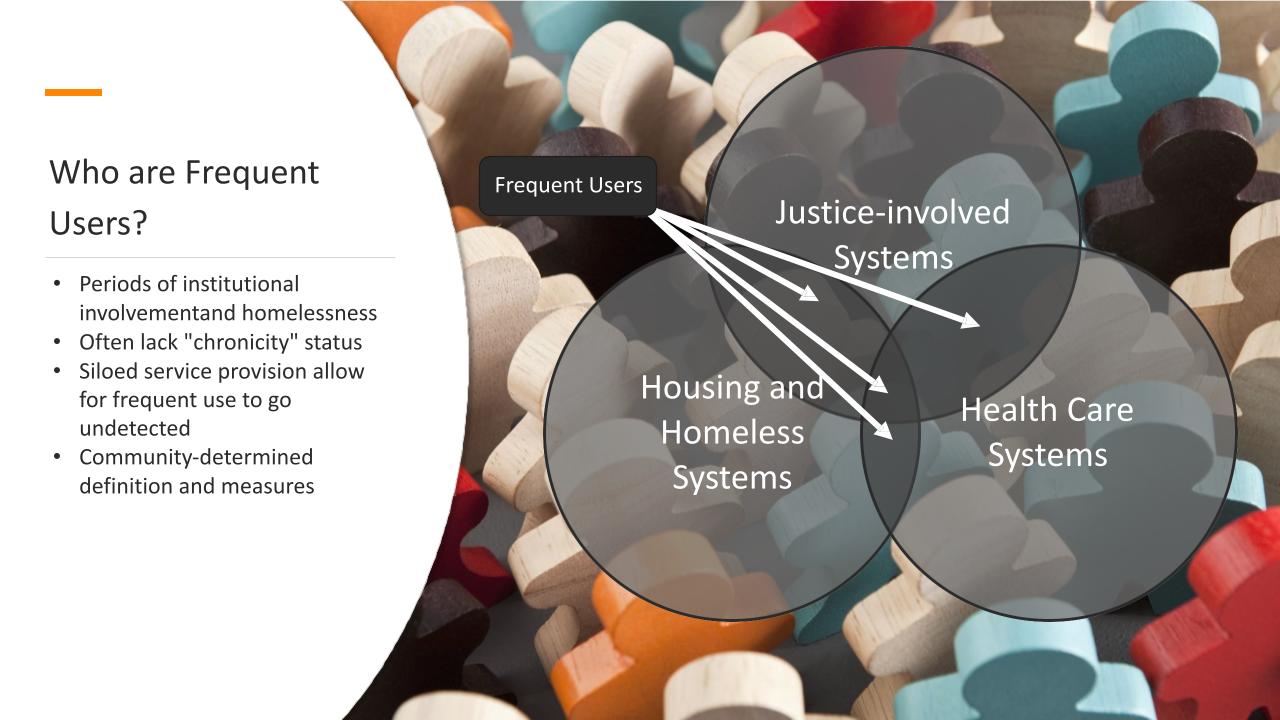
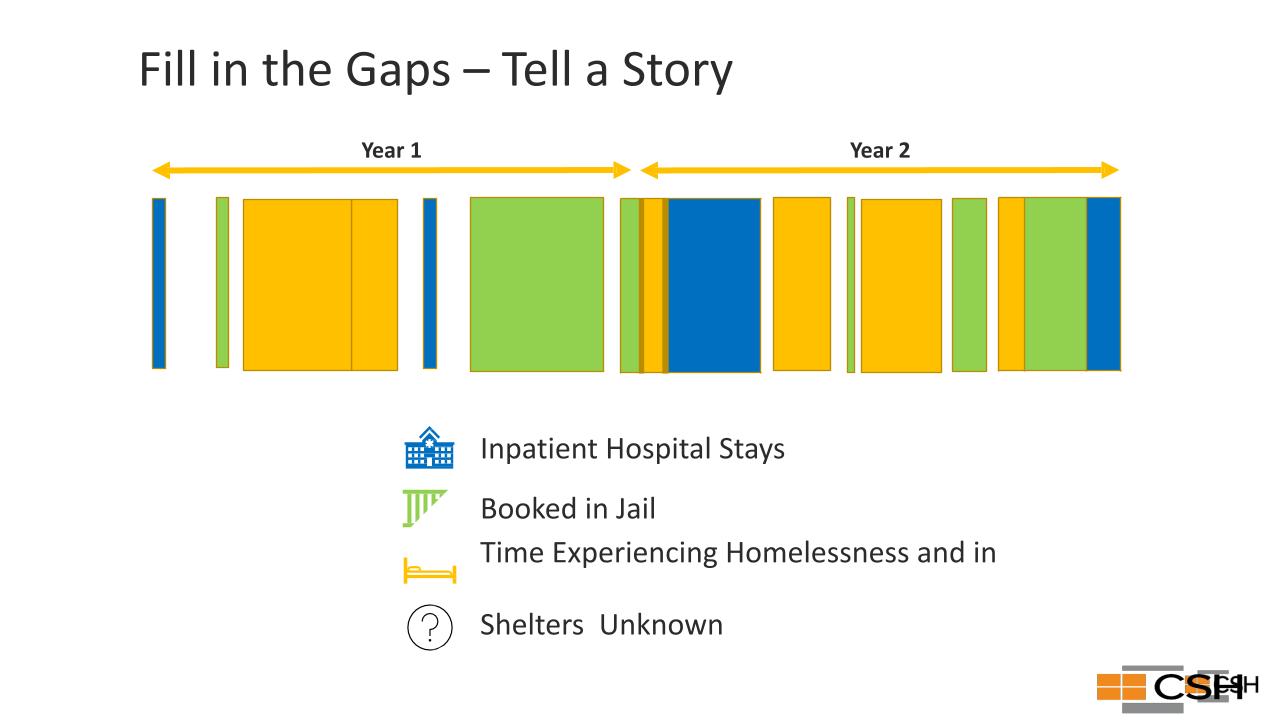
Existing service response systems are high cost and often result in poor outcomes for people who are unsheltered and have multiple experiences with the health care, homelessness response, or justice systems. High-cost and high-need people cycle in and out of these multiple, disconnected and siloed systems.
- People with severe mental illness (SMI), people of color and people struggling with homelessness are overrepresented in jails and prisons.
- People booked into Maricopa County Jail had 3 times the prevalence of SMI in the general population in 2015.
- Among the ~5,000 people with SMI booked, about 50% were homeless.
- In the population of people with SMI and homelessness, individuals tended to be older (average age 38) and people of color (21% were Black/African-American, 12% were Hispanic/Latino, 3% were American-Indian/Alaskan-Native).
- Since the COVID pandemic, rates of people with SMI in jail have escalated with ~10% of people in Maricopa County Jail currently having SMI
Research questions
Can enhancements in coordination of services and multi-sector data matching, lead to sustained improvements in identifying and prioritizing high cost, high need people experiencing homelessness for housing resources and services?
Methods and findings
Adams tested the feasibility of identifying and prioritizing high cost, high need people experiencing homelessness to reduce crisis service utilization and cost to emergency systems. By including people impacted by the justice and health systems in program design and by improving care coordination and data sharing among these systems, this strategy reduces emergency interventions, Impact providing cost savings and better outcomes for people.
Partners
-
Arizona State University
-
Corporation for Supportive Housing
-
Arizona Health Care Cost Containment System (AHCCCS)
-
City of Tucson and Pima County
-
Persons with Lived Expertise
-
Continuum of Care/Homeless Service Providers
-
Law Enforcement/Jail/ Courts
-
Behavioral Health System
-
Emergency Transport System
-
Hospitals/Emergency Rooms
-
Substance Use Treatment System
-
Research/Academia
Impact
Adams aims to scale this pilot up to a statewide program with more than 1,000 supportive housing units. She anticipates that implementing it in two to three states could result in up to 80% housing stability, as well reductions of 25–50% in psychiatric hospitalizations and 30-50% in recidivism. Ultimately, prioritizing high cost, high need populations may support large-scale decriminalization of mental illness may support large-scale decriminalization of mental illness, requiring fundamental changes in the way state and local governments invest resources and reshaping collaboration among health, housing and justice systems.
Margaret Adams
Senior Program Manager
Corporation for Supportive Housing (CSH)
Community Fellow, 2022
With more than 10 years of experience in homelessness and affordable housing policy, I focus on translating complex social problems and helping people and organizations generate solutions to the most urgent issues in their communities. Through education and best practices, I support organizations in envisioning new programs and policies that are equitable and maximize community assets. My deep experience working directly with impacted communities, primarily people experiencing homelessness and justice involvement, guides my work with systems and communities.